Silent sinus syndrome is a rare but significant condition characterized by a spontaneous collapse of the maxillary sinus, leading to various clinical manifestations.
Table of Contents
Introduction
Silent sinus syndrome is a rare but significant condition characterized by a spontaneous collapse of the maxillary sinus, leading to various clinical manifestations. Often unnoticed initially, this syndrome can result in facial asymmetry, double vision (diplopia), and a sunken appearance of the eye (enophthalmos). This article explores the causes, symptoms, and available treatments for silent sinus syndrome, highlighting the importance of recognizing this condition for timely intervention.
What Causes Silent Sinus Syndrome?
Silent sinus syndrome is primarily caused by a failure of ventilation at the osteomeatal complex, which is critical for maintaining healthy sinus function. This condition leads to negative pressure within the maxillary sinus, resulting in its gradual collapse. Key factors contributing to the development of silent sinus syndrome include:
1. Sinusitis: Chronic infection or inflammation of the sinus mucosa can impede normal ventilation, thereby increasing the likelihood of negative pressure.
2. Allergic Rhinitis: Allergies can lead to nasal obstruction, further impacting airflow and drainage of the sinuses.
3. Anatomical Variations: Certain anatomical anomalies, such as a deviated septum or nasal polyps, can obstruct the osteomeatal complex, contributing to the risk of sinus collapse.
4. Prior Surgery or Trauma: Previous surgical interventions in the sinus area or facial trauma may predispose individuals to silent sinus syndrome.
Understanding these causes is vital for healthcare professionals in diagnosing and managing the condition effectively.
Recognizing the Symptoms
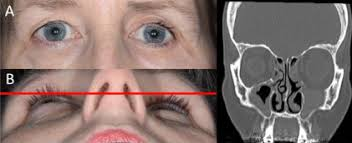
Silent sinus syndrome typically presents with a range of symptoms, often leading to its misdiagnosis. The most common manifestations include:
1. Painless Facial Asymmetry:
- As the maxillary sinus collapses, it can cause noticeable changes in facial symmetry, particularly around the cheeks and eyes.
2. Diplopia (Double Vision):
- Collapse of the sinus may affect the muscles controlling eye movement, leading to double vision or other visual disturbances.
3. Enophthalmos:
- The sunken appearance of the eye occurs due to the downward displacement of the orbital floor as the sinus collapses, contributing to the aesthetic concerns associated with the syndrome.
4. Nasal Obstruction:
- Although not as pronounced, nasal obstruction may be present due to underlying mucus accumulation or inflammation.
5. Facial Pain or Pressure:
- Some patients may experience vague facial discomfort, although this is less common.
Recognizing these symptoms is crucial for early diagnosis and appropriate referral to a specialist.
Diagnosis and Imaging
Accurate diagnosis of silent sinus syndrome typically involves a combination of physical examination, patient history, and imaging studies. Key diagnostic tools include:
1. Clinical Evaluation:
- A thorough physical examination, particularly focusing on facial symmetry and eye movement, is essential.
2. Radiological Imaging:
- CT Scans: High-resolution computed tomography scans of the sinuses are the gold standard for diagnosing silent sinus syndrome, allowing visualization of ostiomeatal complex obstruction and maxillary sinus collapse.
- MRI: In certain cases, magnetic resonance imaging may be employed to assess the extent of orbital involvement.
The combination of physical and imaging assessments aids in distinguishing silent sinus syndrome from other conditions that may present similarly.
Treatment Options
The treatment of silent sinus syndrome typically involves both medical and surgical interventions. Depending on the severity of symptoms and the extent of sinus collapse, options may include:
1. Observation:
- In some cases where symptoms are mild and manageable, a watch-and-wait approach may be appropriate.
2. Surgical Intervention:
- Endoscopic Surgery: The definitive treatment for silent sinus syndrome involves endoscopic intervention to open the osteomeatal complex, restoring ventilation to the sinus.
- Sinus Drainage: In cases of significant mucus accumulation or infection, drainage may be performed to relieve pressure.
3. Postoperative Care:
- Following surgery, patients may require follow-up care to monitor healing and ensure proper sinus function is restored.
Prompt recognition and treatment can significantly improve the prognosis and quality of life for individuals suffering from silent sinus syndrome.
Conclusion
Silent sinus syndrome is a complex condition that can lead to significant facial changes and visual disturbances if left unrecognized and untreated. Understanding its causes, symptoms, and treatment options is essential for healthcare professionals and patients alike. Early diagnosis and surgical intervention can effectively reverse the effects of this condition, restoring both function and aesthetics. As medical knowledge continues to evolve, maintaining awareness of silent sinus syndrome remains crucial for timely and appropriate care.
Tags
syndromes