Patterson–Brown–Kelly syndrome, commonly referred to as Plummer–Vinson syndrome, is a rare disorder primarily affecting middle-aged women.
Table of Contents
Introduction
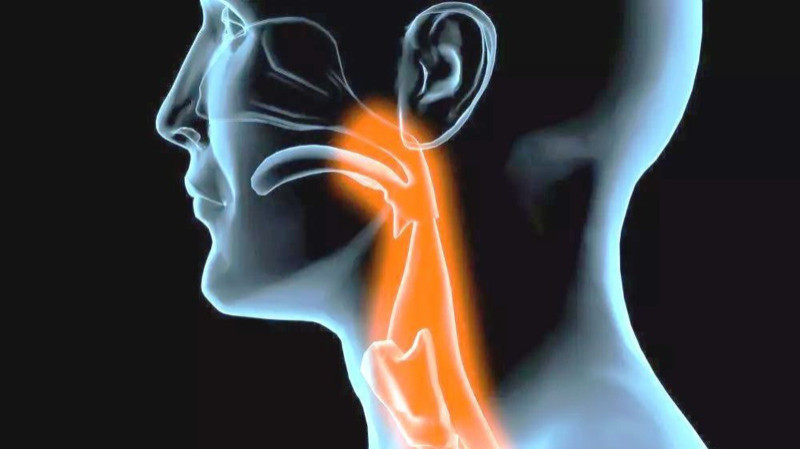
Patterson–Brown–Kelly syndrome, commonly referred to as Plummer–Vinson syndrome, is a rare disorder primarily affecting middle-aged women. Characterized by the triad of dysphagia, microcytic hypochromic anemia, and koilonychia, this syndrome indicates an important intersection of nutritional deficiency and potential malignancy. Usually, the dysphagia observed in patients stems from a web-like membrane formation on the anterior wall of the esophagus, specifically in the post-cricoid region, leading to significant health implications if left untreated. In this article, we will explore the defining features of Patterson–Brown–Kelly syndrome, its causes, symptoms, treatment options, and potential complications.
Key Characteristics
Patterson–Brown–Kelly syndrome manifests through several key symptoms, which may vary in severity among individuals. These include:
- Microcytic hypochromic anemia: A reduced red blood cell volume characterized by smaller-sized cells that lack sufficient hemoglobin, resulting in fatigue and pallor.
- Koilonychia: Spoon-shaped nails that typically follow the onset of anemia, signifying iron deficiency.
- Angular Cheilitis: Cracking and inflammation at the corners of the mouth, making it difficult for individuals to open their mouths fully.
Prevalence and Demographics
Patterson–Brown–Kelly syndrome predominantly affects middle-aged women, typically between the ages of 30 to 60. The condition is notably rare in men and has a higher occurrence in individuals with African descent, indicating a possible genetic or environmental predisposition.
Pathophysiology
Causes
The primary cause of the symptoms observed in Patterson–Brown–Kelly syndrome lies in iron deficiency, often due to:
- Nutritional Deficiencies: Inadequate intake of iron-rich foods, which can lead to anemia.
- Malabsorption Disorders: Conditions such as celiac disease or intestinal infections that impair the body’s ability to absorb nutrients.
- Chronic Blood Loss: Heavy menstrual bleeding or gastrointestinal bleeding from conditions such as ulcers could also contribute to iron deficiency.
Treatment and Management
Addressing the Symptoms
The management of Patterson–Brown–Kelly syndrome focuses on correcting the underlying iron deficiency while addressing the associated symptoms. This includes:
1. Iron Supplementation: Oral iron supplements are typically the first line of treatment to replenish iron stores.
2. Dietary Modifications: Increasing the intake of iron-rich foods such as red meat, spinach, legumes, and fortified cereals can help alleviate symptoms.
3. Management of Dysphagia: In cases where dysphagia is severe, participants may require endoscopic interventions to dilate the esophageal web or surgical procedures to remove it.
4. Monitoring and Follow-Up: Regular follow-up is essential to assess the effectiveness of treatment and to monitor for potential malignant progression of the web, which can occur if the anemia is not adequately addressed.
Complications
Risks and Prognosis
If left untreated, Patterson–Brown–Kelly syndrome carries several risks, including:
- Increased Cancer Risk: The premalignant nature of the esophageal web increases the risk of esophageal squamous cell carcinoma.
- Failure to Thrive: Persistent dysphagia can lead to inadequate nutrient intake and weight loss, impacting the overall health and well-being of the individual.
- Chronic Fatigue: Ongoing anemia can lead to debilitating fatigue and affect the quality of life.
However, with early diagnosis and proper treatment, the prognosis for Patterson–Brown–Kelly syndrome can be favorable. Correcting the anemia often leads to the alleviation of dysphagia and can effectively prevent the malignant progression associated with the esophageal web.
Conclusion
In conclusion, Patterson–Brown–Kelly syndrome presents several significant health concerns, specifically dysphagia, iron deficiency anemia, koilonychia, and angular cheilitis, mostly affecting middle-aged women. Understanding the underlying causes and implementing appropriate treatment strategies are crucial in managing the symptoms effectively and preventing possible complications. As awareness grows surrounding this rare syndrome, timely intervention becomes pivotal, ultimately enhancing patients' quality of life and reducing the risks associated with esophageal malignancy. As we continue to unpack the complexities of Patterson–Brown–Kelly syndrome, there remains a crucial need for ongoing research and education regarding its symptoms, treatment, and long-term management.
Tags
syndromes