Peutz–Jeghers syndrome (PJS) is an autosomal dominant genetic disorder characterized by distinct clinical features, including melanotic pigmentation and intestinal polyposis.
Table of Contents
Introduction
Peutz–Jeghers syndrome (PJS) is an autosomal dominant genetic disorder characterized by distinct clinical features, including melanotic pigmentation and intestinal polyposis. This rare condition affects various aspects of an individual’s health, presenting unique challenges in diagnosis and management. In this article, we will explore the fundamental aspects of Peutz–Jeghers syndrome, focusing on its symptoms, related health risks, and management strategies.
Key Features of Peutz–Jeghers Syndrome
-- Melanotic Pigmentation
One of the hallmark features of PJS is the emergence of pigmented spots on the skin and mucosal surfaces. Key characteristics include:
- Location: These lesions are particularly prominent around mucosal areas, especially the peri-oral skin, but may also appear on the fingers and toes.
- Appearance: The pigmentation tends to be dark brown to blue in color and is often café-au-lait-like in appearance.
- Development: These spots usually appear during early childhood and increase in frequency and intensity over time.
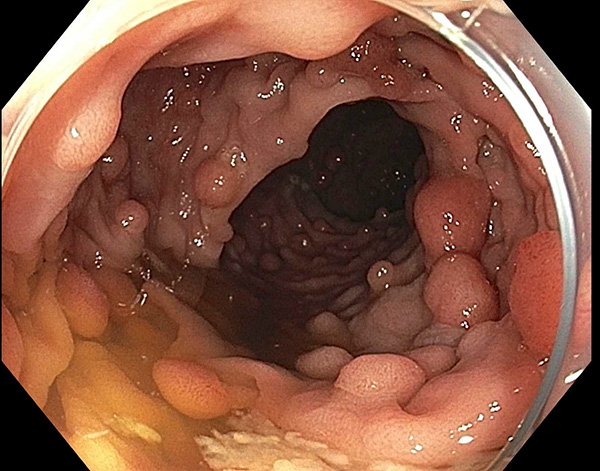
-- Intestinal Polyposis
Individuals with Peutz–Jeghers syndrome typically develop multiple hamartomatous polyps in the gastrointestinal tract, especially within the small intestine. Important details include:
- Types of Polyps: Unlike the adenomatous polyps seen in other types of syndromes, the polyps in PJS are benign hamartomas that carry no significant risk of malignant transformation.
- Complications: Despite their benign nature, these polyps can lead to serious gastrointestinal complications, including:
- Intussusception: A condition where a part of the intestine telescopes into itself, potentially causing blockage.
- Obstruction: Symptoms may arise from obstructed bowel due to large polyps or intussusception, necessitating medical intervention.
Associated Health Risks
While Peutz–Jeghers syndrome primarily manifests through pigmentation and polyps, it carries several associated health risks that patients and healthcare providers must be aware of. Notable associations include:
1. Ovarian Tumours
- Women with Peutz–Jeghers syndrome have approximately a 10% risk of developing ovarian tumours. These can include sex-cord stromal tumors, which may often be benign but can lead to serious health concerns.
2. Increased Cancer Risk
Although the hamartomas associated with PJS are benign and do not exhibit malignant potential, individuals with this syndrome have an increased risk of developing certain types of cancer over their lifetime. Among them are:
- Gastrointestinal cancers (including gastric and colorectal cancers)
- Breast cancer
- Pancreatic cancer
While the precise increase in risk varies, the need for regular surveillance and management is emphasized.
Diagnosis and Management
Diagnosing Peutz–Jeghers syndrome primarily involves clinical evaluation and genetic testing. Key steps are as follows:
1. Clinical Evaluation
- Family History: A comprehensive family history can reveal patterns consistent with an autosomal dominant inheritance.
- Physical Examination: Identification of characteristic pigmented lesions and intestinal polyps through endoscopic or radiologic studies.
- Genetic mutation analysis can confirm the diagnosis of PJS, with mutations typically identified in the STK11/LKB1 gene.
3. Management Strategies
- Surveillance: Regular gastrointestinal surveillance is crucial to monitor the development of polyps and identify any potential complications early.
- Surgical Intervention: In cases where polyps lead to obstruction or other complications, surgical removal may be necessary.
- Referral to Specialists: Patients may benefit from a multidisciplinary approach involving gastroenterologists, gynecologists, and genetic counselors to optimize management.
Conclusion
Peutz–Jeghers syndrome is a complex genetic condition with significant clinical and health implications. The combination of distinctive skin pigmentation and intestinal polyposis necessitates awareness and appropriate management strategies to mitigate associated risks, particularly the potential for gastrointestinal obstructions and other cancers. Ongoing research and patient education will be vital in enhancing the understanding and treatment of this syndrome, ensuring better health outcomes for those affected. As we advance in our understanding of genetic disorders, the importance of early diagnosis and interdisciplinary care becomes increasingly evident in managing Peutz–Jeghers syndrome effectively.
Tags
syndromes